Health

Health
Artificial Intelligence Rewrites the Rules of Diabetes Management: Cleveland Clinic Breakthrough
In the fight against Type 2 diabetes, a chronic disease affecting nearly 38 million Americans, a new powerful ally has emerged: artificial intelligence. An innovative study by Cleveland Clinic, published in the journal New England Journal of Medicine Catalyst, demonstrates how an AI-based program can radically change the approach to blood sugar control by offering a personalized alternative to traditional treatment methods.The program, developed by Twin Health and named Twin Precision Treatment, utilizes cutting-edge technologies — from wearable sensors to Bluetooth devices — to monitor key health indicators such as glucose levels, weight, blood pressure, physical activity, and sleep. These data are analyzed in real time by artificial intelligence, which generates individualized recommendations for nutrition and physical exercise, available through a convenient smartphone app. The uniqueness of the program lies in its ability to predict the body's response to specific foods and adjust recommendations according to each patient's metabolism.“Type 2 diabetes isn’t a disease that can be treated with a one-size-fits-all approach,” notes Dr. Kevin M. Pantalone, director of the Cleveland Clinic’s Diabetes Initiative and lead researcher of the project. “Our goal is to understand the unique needs of each patient. This program allows us not only to improve diabetes control but also to reduce dependence on medications, which is a real breakthrough.”The study results are impressive: 71% of participants using Twin Precision Treatment achieved an A1C (average blood sugar level) below 6.5%, while taking only metformin — a standard medication for diabetes. In comparison, only 2.4% of patients receiving traditional treatment reached a similar result. Additionally, participants lost more weight and significantly reduced their use of additional glucose-lowering medications.The study involved 150 patients with an average age of 58.5 years, who had been battling Type 2 diabetes for an average of nine years. At the start, their A1C level was 7.2%, indicating moderate disease control. However, Twin Health’s program proved that a personalized approach can fundamentally change the situation, offering not only medical benefits but also psychological advantages, as participants felt greater control over their health.According to the U.S. Centers for Disease Control and Prevention, diabetes affects about one in ten Americans, with 90% of cases being Type 2 diabetes. Uncontrolled blood sugar levels increase the risk of heart disease, kidney failure, stroke, and premature death. Against this alarming backdrop, Cleveland Clinic’s breakthrough is particularly significant, offering not just hope but a practical solution for millions of people.Healthcare insiders note that the success of Twin Precision Treatment could herald a new era in the treatment of chronic diseases. “This is not just technology,” remarks one leading endocrinologist who wished to remain anonymous. “It’s a paradigm shift that puts the patient at the center of the medical process.” However, questions remain about the accessibility of such technology: whether insurance companies and government programs like Medicare will cover its use for a broader audience.While these issues are still unresolved, one thing is clear: artificial intelligence already not only promises but is actively changing people's lives. For those battling Type 2 diabetes, this study is a beacon of hope pointing toward a future where technology and human care unite to create a healthier world.
18.09.2025
Health
Ohio stands guard over science: The state rejects the anti-vaccine shift, unlike Florida
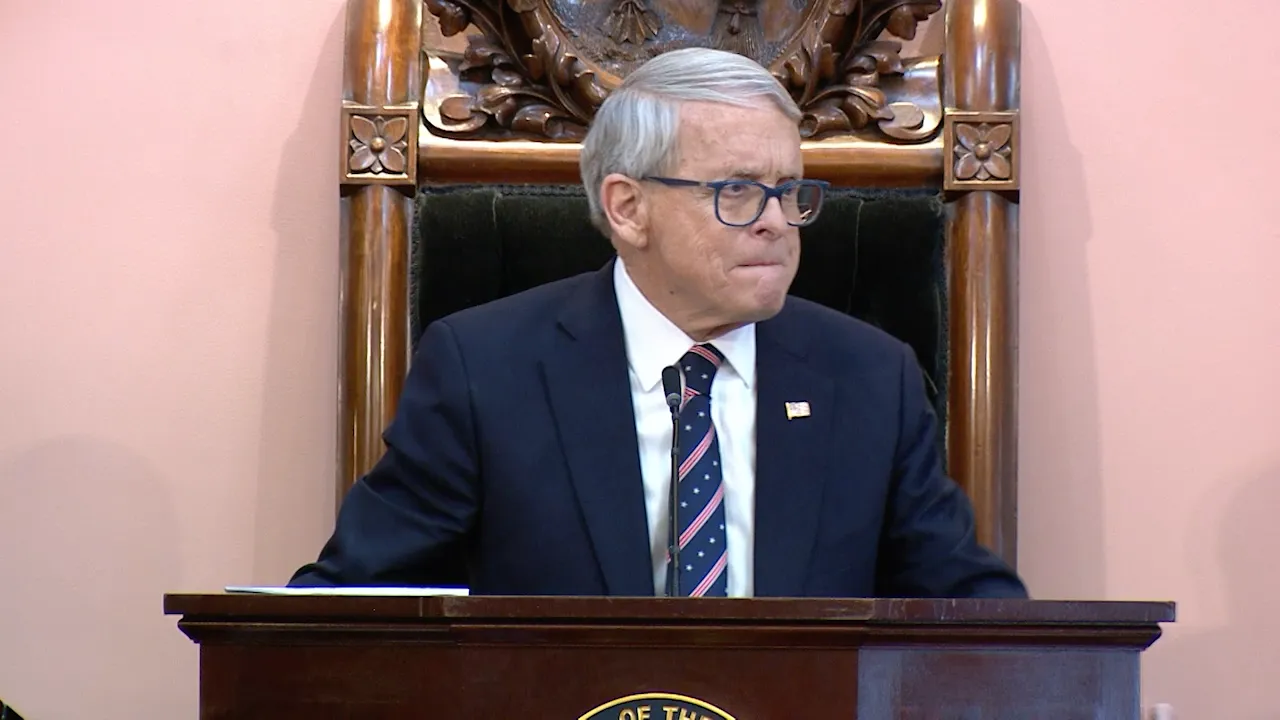
In times when political winds in Washington blow toward skepticism regarding vaccines, Ohio chooses a path paved by decades of scientific evidence rather than ideological whims. In contrast to Florida, which actively promotes legislation for a complete ban on vaccination requirements, Republican Governor Mike DeWine and his team at the Ohio Department of Health have clearly stated: the state will continue to promote the benefits of immunization as a key public health tool. This approach seems to be a rare island of rationality in a landscape where anti-vaccine rhetoric is gaining momentum under the influence of the Trump administration.
According to internal sources in the governor's office, DeWine and Department Director Dr. Bruce Vanderhoff remain steadfast in their commitment to scientific data. "We will not allow political speculation to undermine the health of our citizens," emphasized one of the governor's advisors, who requested anonymity due to the sensitivity of the topic. This stance contrasts with recent statements by Secretary of Health and Human Services Robert F. Kennedy Jr. during congressional hearings, where he claimed that "many vaccines do more harm," a assertion unanimously refuted by leading medical experts, including the American Medical Association and the Centers for Disease Control and Prevention (CDC). Kennedy Jr., known for his longstanding anti-vaccine campaigning, not only halted funding for the development of new vaccines but also dismissed key CDC officials, stating: "We are the sickest country in the world, so we need to fire people at CDC. They didn't do their job."
In Ohio, where the balance of power in the legislature barely leans toward Republicans, this tension is evident at every turn. The percentage of vaccinated children entering kindergarten continues to decline — from 89.9% in the 2019-2020 school year to 85.4% today, a decrease of 4.5% over five years. This trend reflects a national pattern where outbreaks of diseases such as measles and mumps are becoming more frequent due to the spread of misinformation on social media and political circles. However, not everyone in Ohio shares this concern. State Representative Bet Liston, a Democrat from Dublín and a seasoned pediatrician, exemplifies an opposite approach. "I do all available vaccinations for my children," she said in an interview I conducted at her office. Liston, who has witnessed the consequences of the anti-vaccine movement firsthand in her practice, warns: "There are many diseases we can prevent, and many health problems, including death, that would arise if we didn't have vaccines." Her words resonate with insider assessments from CDC experts who, despite staffing reductions, continue to document how vaccination has saved millions of lives globally since Ernst von Schark, a pioneer of immunization.
However, the "Make America Healthy Again" campaign, inspired by Trump and Kennedy Jr., has found resonance in Ohio. Bill No. 112, initiated by Representative Jennifer Gross (Republican from West Chester), prohibits discrimination against individuals refusing vaccination and is nearly identical to her initiative from last year. Sponsor Bet Lierst, another Republican legislator, argues: "When states, including Ohio, began requiring unverified and unproven mRNA vaccinations as a condition of employment and education, I and many others in the state and country realized that the government was intervening too much." Gross, who actively supports Florida's efforts to fully ban mandates — even for schoolchildren — stated in 2024: "Ohio residents are forced to abandon their conscientious or religious beliefs or face the reality that they cannot be productive members of our society." Lierst adds: "If vaccines are truly safe and effective, they will be in high demand and there will be no need for mandatory requirements."
According to Liston, these arguments are a direct consequence of misinformation. "Misinformation leads to a lack of demand," she notes, citing numerous studies published in "The Lancet" and "New England Journal of Medicine" that confirm the safety and efficacy of COVID-19 vaccines, including mRNA technologies. Doctors nationwide, including those I have spoken with privately, constantly assert: these vaccines have undergone rigorous testing, have saved millions of lives, and do not pose systemic risks.
Meanwhile, other states are reacting to federal pressure. California, Oregon, Washington, and Hawaii have formed a coalition to disseminate "reliable information" and counter the Trump administration, while northeastern states like Massachusetts, according to Governor Maura Healey, are preparing their own alliance. Ohio, however, remains on the sidelines. "We acted Ohio-style and issued Ohio recommendations," said Ohio Governor's spokesperson, Dan Terny, emphasizing the state's autonomy. "You often hear that Ohio politicians want to act 'Ohio-style' and not necessarily join, replacing and weakening the power of Ohio residents by handing it over to a multi-state conglomerate."
Liston, perceiving a party divide in this, appeals for unity: "Science should not be a partisan issue. We all want children to be healthy; we all want to use the best evidence in society to achieve better health outcomes. I believe division and distrust are regrettable." Her words echo insider assessments from Capitol Hill: in private conversations with Ohio legislators, anti-vaccine initiatives are often seen as tactical moves to mobilize the base but face resistance from moderate Republicans like DeWine, who has repeatedly vetoed similar bills citing public health interests.
Ultimately, Ohio is becoming a testing ground for America: will science outweigh populism? Given the governor’s history as a long-time advocate for children's well-being, Bill No. 112 is likely to face a veto — a signal that even in the heartland "rust belt" states, there is still room for a rational voice. As my sources in the medical community suggest, this could become a model for other Republican states that are torn between ideology and epidemiology.
12.09.2025

Health
Ohio aims to ban sugary drinks in the SNAP program: an ambitious move or a bureaucratic trap?
A new initiative is unfolding in Ohio that could change how 1.4 million residents use their food stamps. Governor Mike DeWine, known for his cautious support of health care reforms, has created a special working group to pave the way for a ban on the use of the Supplemental Nutrition Assistance Program (SNAP) for purchasing sugary beverages. This move, aimed at combating obesity and related health conditions, has garnered both support and concern among experts, retailers, and social advocates.This week, the newly formed working group, composed of senior officials, health experts, and industry representatives, will convene in Columbus to develop a federal request to waive existing SNAP regulations. This request, which must be submitted to the U.S. Department of Agriculture (USDA) by October 28, is a crucial step toward enacting a ban similar to the one recently approved in Indiana. However, the path to change has proven to be thorny, as DeWine vetoed an earlier legislative attempt to include this ban in the state budget, citing its excessive complexity."We’re not opposed to the idea of restricting low-nutrition foods," DeWine said at a press conference earlier this month, "but the language in the bill created more problems than it solved." His concerns reflect broader debates: how to balance public health concerns with the practical realities of administering a large-scale social program that affects a significant portion of Ohio’s population?The Complex Mission of the Working GroupThe working group, which includes key figures such as Matt Damschroder, Director of Ohio’s Department of Jobs and Family Services, and Bruce Vanderhoff, Director of the Department of Health, is tasked with providing recommendations by September 28 regarding the form and scope of the ban. Industry representatives are also involved, including Kimberly McConville from the Ohio Beverage Manufacturers Association and Christine Mallins from the Food Retailers Association. Their presence highlights the delicate balance between public health interests and economic realities in retail.McConville, who shares Governor’s concerns about the draft language, expressed cautious optimism. "This working group has a chance to develop a sensible pilot program that includes clear metrics for evaluating health impacts and transparent accounting of costs," she said in an interview with Cleveland.com. Her words reflect a desire for an evidence-based approach, which is rare in a politically charged environment of social reform.However, not all are so optimistic. Critics, including advocates for the rights of the poor, argue that restricting food choices within SNAP could stigmatize benefit recipients and complicate access to nutritious foods for low-income families. "It sounds like health concern, but in practice, it could become just another barrier for those already struggling to survive," said Sarah Jones, director of a local charity fighting poverty, who is not part of the working group.Federal Challenges and Broader ContextThe idea of banning sugary drinks in SNAP is not new, but it faces serious hurdles. USDA, which oversees the program, has historically been skeptical of such restrictions, citing administrative complexity and concerns over recipients’ freedom of choice. Approving such a ban in Indiana in May was a rare exception, and Ohio hopes to replicate that success. However, insiders say federal approval depends on a clear justification backed by data on health benefits and economic feasibility.This initiative also reflects broader national debates about the role of government in regulating citizens’ diets. While some see banning sugary beverages as a necessary step in combating the obesity epidemic, others view it as paternalistic overreach. Research from the Public Decision-Making Center, represented in the working group by Rachel Keihill, indicates that sugary drinks account for a significant portion of calories consumed by SNAP participants but offer little nutritional value. Still, whether a ban will lead to real health improvements remains an open question.What’s Next?The first meeting of the working group will take place on Thursday at the Rhodes State Office Tower in Columbus, alongside another initiative by DeWine — a working group on property tax reform, which is also co-chaired by Pat Tiberi. This coincidence highlights the governor’s ambitious agenda, aiming to address health, economic, and social policy issues simultaneously.Whether Ohio can successfully implement this ban depends on the group’s ability to navigate bureaucratic and political obstacles. For DeWine, whose administration often balances progressive reforms and conservative caution, this initiative is a test of his capacity to turn complex ideas into action. For Ohio’s 1.4 million residents dependent on SNAP, the implications could be much more profound — and not necessarily positive.
01.08.2025

Health
Popular YoCrunch yogurt recalled due to plastic contamination: what consumers need to know
The U.S. Food and Drug Administration (FDA) announced a major recall of the popular yogurt YoCrunch, sold in retail chains such as Walmart, due to the detection of plastic fragments that pose a serious health risk to consumers. This step has raised concerns among shoppers and brought into question the quality control in the food industry, which has far-reaching implications for brand trust.
The recall, initiated by Danone U.S., concerns a wide range of YoCrunch yogurt flavors, including consumer favorites such as "Strawberry with Granola," "Vanilla with M&Ms," and "Vanilla with Oreo." The issue is related to plastic caps used for packaging the fillings, where, according to reports from consumers, foreign fragments have been found. The FDA warns that these plastic pieces can cause oral injuries or even pose a choking hazard, making the situation especially troubling for families with children who often choose these brightly packaged yogurts.
The scale of the problem
The recall covers both 6-ounce single-serving cups and multi-pack sets with expiry dates from July 7, 2025, to September 4, 2025. According to sources close to Danone, the problem arose due to a malfunction on one of the production lines, where defective equipment led to plastic particles contaminating the packaging. Although Danone responded promptly, working with the FDA to remove the products from shelves, the incident has already sparked a wave of criticism on social media, where consumers share photos of plastic fragments found in the yogurts.
"This is unacceptable," — says Emily Carter, a mother of two from Philadelphia who found a plastic fragment in a yogurt purchased for her daughter. "We trust these brands, and they are endangering our children." Her comment reflects broader concern: how did one of the leading companies in the food industry allow such an error?
The company's reaction and further actions
Danone U.S. issued a statement apologizing for the inconvenience and reassuring consumers that measures are being taken to address the problem. "The safety of our customers is our top priority," the company's statement reads. "We are working with retail chains to swiftly remove affected batches from sale." The company also urged consumers to check batch codes on packages and return the products to stores for a refund.
However, for many, this may not be sufficient. The YoCrunch incident adds another item to the list of recent food recalls, prompting industry experts to question the effectiveness of quality control systems. "Such cases undermine brand trust and can have long-term impacts on sales," notes Dr. Linda Harris, a food safety expert at the University of California, Davis. She adds that companies should invest in more advanced foreign object detection technologies to prevent such incidents.
What should consumers do?
The FDA advises consumers to check the batch codes on YoCrunch packages and immediately cease consumption of products from the specified batches. Walmart and other retail chains have already begun removing yogurts from the shelves, and some stores have posted warning notices. Consumers can contact Danone's hotline for additional information or a refund.
This incident also serves as a reminder of the importance of consumer vigilance. "Always check products before consumption, especially if they are intended for children," recommends Dr. Harris. While Danone and the FDA work to resolve the situation, thousands of American families are reviewing the contents of their refrigerators, questioning whether they can trust their favorite products.
29.07.2025

Health
Toxic Ohio Strike: Air Quality Advisory Sparks Alarm in the Northeast
North-eastern Ohio has found itself in the choking grip of an air quality alert issued by the Northeast Ohio Areawide Coordinating Agency (NOACA), signaling a growing environmental crisis threatening the health of vulnerable populations. By midnight on Monday, counties Ashland, Cuyahoga, Geauga, Lake, Lorain, Medina, Portage, and Summit will be under this warning, highlighting the fragility of the balance between industrial progress and community health.It is expected that air quality in these counties will reach levels hazardous for sensitive groups — children, the elderly, and those suffering from respiratory conditions such as asthma or chronic obstructive pulmonary disease. According to AirNow.gov, which monitors real-time air quality, pollutant concentrations, including ozone and fine particulate matter, may make breathing difficult and exacerbate existing health problems. Residents are advised to limit outdoor activities, especially during peak pollution hours, and regularly check official sources for updates.Root CausesNortheastern Ohio, an industrial hub with a rich history of steel manufacturing and energy production, has long struggled with air quality issues. Insiders from NOACA, who wished to remain anonymous, point to a combination of factors: stagnant weather conditions that trap pollutants, emissions from coal-fired power plants and transportation sectors, and seasonal increases in activities like lawn mowing and car refueling during hot weather. These sources, although routine, create a toxic cocktail that threatens public health."It’s not just weather or industry — it’s a systemic problem requiring collective responsibility," said one local environmental activist working with regional authorities. However, for many residents, especially in working-class communities dependent on industrial jobs, calls to reduce emissions sound like a distant utopia.Call to ActionNOACA and environmental agencies strongly urge residents to take measures to reduce pollution. The recommendations are simple but impactful: favor biking or walking, use public transportation, work from home if possible, and avoid solo car trips. Turning off engines when idling, refueling after sunset, and refraining from lawn mowing during alerts can also help. Although these actions may seem minor, they are critical for reducing ground-level ozone, which forms under sunlight and emissions.Global Context, Local ImpactThe Ohio warning reflects a broader national trend. According to the U.S. Environmental Protection Agency (EPA), air quality in many regions is worsening due to climate change, which amplifies heatwaves and stagnant air conditions. In 2024, the EPA reported that over 120 million Americans live in areas with periodically hazardous air pollution levels. For Ohio, where industry and transportation remain economic pillars, this issue takes on particular significance.Residents of Cleveland and nearby towns such as Akron and Youngstown feel it firsthand. "I see my kids coughing after playing outside," says Maria Gonzales, a mother of two from Lorain. "We can’t just stay at home all the time, but what can we do?" Her words reflect the frustration of many who feel trapped by circumstances.Looking to the FutureEnvironmental experts and officials agree that temporary measures like limiting outdoor activities are only short-term solutions. Long-term changes will require investments in cleaner energy sources, modernization of public transportation, and stricter regulations for industrial facilities. However, Ohio’s political climate, where economic priorities often outweigh environmental concerns, makes rapid progress difficult.As the region prepares for yet another day of choking air, the call to action is clear: individual efforts, multiplied by thousands, can make a difference. But is that enough to clear the skies over Ohio? The answer depends on whether communities, industry, and government are willing to unite for one shared goal — clean air for all.
28.07.2025

Health
Tragedies on Ohio Lakes Prompt Changes: Petition for Safety at Portage Lakes State Park
In Portage Lakes State Park, where picturesque lakes attract thousands of visitors every summer, tragedies in recent years cast a shadow over this natural paradise. Following several drowning incidents, including the recent death of a 49-year-old man from Akron on June 24, local resident Cory Evans launched a campaign to improve safety in the park. His increasingly popular petition calls for decisive changes — from clearer signage and fencing to increased numbers of lifeguards — to save lives and make the park safer for everyone.
Portage Lakes, located just a few miles from Akron’s industrial heart, has long been a favorite spot for families, anglers, and water recreation enthusiasts. On a hot Tuesday, when temperatures reached 29°C, park beaches buzzed with children’s laughter and the splash of waves. “It’s a little slice of heaven,” says Evans, who grew up swimming in these waters. But for him and many others, the joy of recreation is overshadowed by concerns over safety measures.
“If we can save even one life, it will be worth it,” emphasizes Evans, whose personal experience — losing his uncle in a frozen lake accident — motivated him to take action. His online petition calls for the installation of clear warning signs, improved fencing around swimming areas, hiring additional lifeguards and rangers, and educational programs about water safety. Evans has already discussed these ideas with local legislators, hoping that funding for these initiatives will be included in the next state budget.
Local visitors share his concerns. Patrick Smith, a resident of Green who brought his grandchildren to the beach, notes: “There are no lifeguards here, so you’re swimming at your own risk. I closely watch over the kids.” Similarly cautious is Ben S., a father of three from Michigan, who insists that his younger children always wear life jackets. “We love this place, but safety comes first,” he says.
The recent drowning incident on June 24, when a man went underwater near the park’s main beach and his body was only found hours later, served as a tragic reminder of the risks. The Franklin Fire Department confirmed that this is not the first such incident in the park. The lack of lifeguards and inadequate safety infrastructure raise increasing public concern.
The Ohio Department of Natural Resources (ODNR), responding to inquiries, stated that safety is their “top priority.” A spokesperson emphasized the importance of safe swimming rules, such as wearing life jackets and supervising children. However, critics, including Evans, believe these recommendations are only half-measures that do not address systemic issues like staffing shortages or outdated infrastructure.
Evans’s petition is not just a call for change but also an attempt to reimagine how Ohio cares for its natural treasures. “This park can be safer and more inviting for everyone,” he says. “We must act before another tragedy occurs.” In a state where public parks are an economic and cultural asset, raising awareness about safety could serve as an example for other regions facing similar challenges.
As the petition gains support and families continue to enjoy sunny days on the lakes, the question remains: can Ohio find a balance between preserving the natural beauty of Portage Lakes and protecting those who come here for recreation? For Evans, the answer is clear: “Safety is an investment in the future of this place.”
19.07.2025

Health
The US is experiencing the worst year in three decades due to a measles outbreak
The United States has found itself at the epicenter of the worst measles outbreak in the last three decades, and this is only mid-year. According to the Centers for Disease Control and Prevention (CDC), as of July 2025, the country has recorded 1,288 cases — a figure that surpasses the record set in 2019, when America nearly lost its status as a measles-free country. Experts warn: if the virus continues to spread unabated throughout the year, this status could be lost permanently.
This crisis, according to healthcare professionals, is not only a medical but also a social catastrophe, reflecting deep-rooted issues in attitudes toward vaccination. "It's like a canary in a coal mine," notes Lauren Gardner, head of the measles tracking database at Johns Hopkins University. "We see a problem that is likely to only worsen."
Record Numbers and Human Losses
According to CDC data, the current outbreak exceeds the 2019 figures by 14 cases but is still far from the peak of 1991, when 9,643 cases were registered. However, the tragedy has already claimed three lives: two children in West Texas and one adult in New Mexico. Dozens were hospitalized. The largest outbreak, which began five months ago in communities with low vaccination rates in West Texas, has revealed systemic gaps in healthcare.
Katherine Wells, director of the Lubbock County Department of Health, reported that there have been no new cases in her region for the past 50 days, offering cautious optimism. "But I am concerned that the virus is already spreading to other parts of the country," she added. Active outbreaks have been recorded in 14 states, while in four others they have recently subsided.
Vaccination: Available but Rejected
Measles is a disease preventable with the MMR vaccine (measles, mumps, rubella), which has 97% effectiveness after two doses. In 2000, the World Health Organization and CDC declared that measles had been eliminated in the USA. However, today, despite widespread availability of vaccines, the return of the disease causes a sense of "melancholy" among medical professionals, according to Dr. Jonathan Temte, a family physician from Wisconsin who helped confirm this achievement 25 years ago.
CDC data from 2023–2024 shows that only 92.7% of preschool children in the USA received the MMR vaccine — below the critical threshold of 95% needed to prevent outbreaks. After the COVID-19 pandemic, the vaccination rate among children against measles fell by nearly 80% in over 2,000 districts where data is available. "When we have an effective tool but people reject it without valid reasons, it’s frustrating," Temte noted.
Outbreaks in Texas, as well as in Chihuahua (Mexico, 2,966 cases), Ontario (Canada, 2,223 cases), and Alberta (Canada, 1,246 cases), are linked to communities with low vaccination rates, notably Mennonite communities. While Mennonite churches officially do not oppose vaccination, conservative communities historically demonstrate distrust of government initiatives and have low immunization levels. A similar situation was observed in 2019, when outbreaks in New York were linked to Orthodox Jewish communities.
Wells emphasizes the chronic underfunding of vaccination programs. "Local health departments do everything possible, but without adequate resources, we cannot change this trend," she said. According to her, significant investments in healthcare infrastructure are needed to stop the spread of the disease.
Looking to the Future
The current measles crisis is not only a medical challenge but also a mirror reflecting broader societal issues — distrust in science, misinformation, and insufficient funding of public health. If urgent measures are not taken, the USA risks losing its status as a measles-free country, which could have far-reaching consequences for the nation’s health.
"We have a vaccine that works, but we cannot force people to use it," Gardner summed up. "This is a fight not only against a virus but also against convictions."
16.07.2025

Health
Community Heroes: MetroHealth Leads the Rankings of Socially Responsible Hospitals in Northeast Ohio
CLEVELAND, Ohio — While American healthcare grapples with economic hardships and rising inequality, four hospitals in Northeast Ohio stand out as beacons of social responsibility. According to the Lown Institute’s Hospital Social Responsibility Index for 2025-2026, MetroHealth System leads the region, ranking 36th nationally, followed by Cleveland Clinic South Pointe (41), Summa Health Akron (95), and UH Portage Medical Center (102). These institutions, recognized among the top 125 in the “Honor Roll” list out of more than 2,700 intensive care hospitals nationwide, demonstrate how healthcare facilities can go beyond clinical excellence to strengthen the communities they serve. In a state where economic challenges and disparities in healthcare access remain acute, their work is more relevant than ever.The Lown Institute, an unbiased analytical center in Boston, evaluates hospitals based on over 50 indicators covering fairness, value of care, and patient outcomes. The ranking, published on June 24, 2025, relies on data from Medicare, the U.S. Internal Revenue Service, and other sources to assess how hospitals invest in communities, avoid excessive procedures, and provide inclusive care. “High-value healthcare is only meaningful when it is accessible to all,” said Vikas Saini, president of the Lown Institute. “These hospitals show what it truly means to be a community partner.”MetroHealth: A Leader with a Human FaceMetroHealth, ranked on the “Honor Roll” for the fourth consecutive year, received the highest “A” grades for fairness, value, and outcomes, ranking second among Ohio hospitals and first in categories such as “community benefit” and “avoidance of overuse.” Its initiatives, including the School Health Program, which provides medical services in over 25 schools in Cuyahoga County, and partnerships with the Northeast Ohio Coalition for the Homeless, highlight its commitment to vulnerable populations. The BREAST/Amigas Unidas program, a bilingual initiative aimed at educating Latina women about breast cancer, exemplifies culturally sensitive community health approaches. “No other hospital in America has a more dedicated staff,” declared Michelle Alexander-Reger, President of MetroHealth, emphasizing that their mission — “hope, health, and humanity” — underpins every action.Despite a $4.6 million deficit in 2024 due to increasing uncompensated care and staffing shortages, MetroHealth continues to expand its initiatives, including a new outpatient center opening in 2026 and a pharmacy in Brooklyn to improve access to medications. These efforts contrast with the broader picture in Ohio, where many hospitals face financial difficulties but not all invest as generously in their communities.Cleveland Clinic South Pointe: Listening to the NeighborsCleveland Clinic South Pointe, ranked 41st nationally, has been named to the “Honor Roll” for the second time. Located in Warren'sville Heights, this hospital was recognized for its efforts toward equitable access to care and avoiding unnecessary procedures. Programs such as a $52.5 million investment to eliminate lead contamination in Cleveland homes and mentorship initiatives for local entrepreneurs from underrepresented groups reflect its social impact ambitions. “We are transforming communities by listening to our neighbors and collaborating with partners,” said Cleveland Clinic, emphasizing its holistic partnership approach.However, despite its reputation for clinical excellence, the main Cleveland Clinic campus ranked fifth among 20 American hospitals with the poorest community cost-to-benefit ratio relative to received tax benefits, prompting criticism about its “fair contribution.” This contrast highlights the gap between clinical achievements and social responsibility, a focal point of the Lown methodology.Summa Health Akron: Three Years of RecognitionSumma Health Akron, ranked 95th, has made the Honor Roll for the third time, demonstrating consistent community commitment. Its programs, such as mentoring Black students aspiring to medical careers and investments in preventive screenings, have received praise. “This recognition reflects the compassionate care our staff provides every day,” said Iriel Hopkins, Director of Community Relations. Despite an $8 million operating loss in 2024, Summa remains a leader in the Akron market, though its upcoming merger with venture firm General Catalyst, valued at $485 million and expected to finalize in mid-2025, raises concerns about future healthcare accessibility.UH Portage: A New Name in the RankingsUH Portage Medical Center in Ravenna, ranked 102nd on its first appearance on the “Honor Roll,” is distinguished by initiatives focused on pregnant women and fighting food insecurity. A mobile diagnostic center for obstetric ultrasounds and free farmers’ markets in three low-income areas, in partnership with Kent State University, help families access healthy foods and education. “We are investing in our communities’ future,” states UH, highlighting its focus on social determinants of health. However, the main UH Cleveland Medical Center ranked sixth in Ohio for the poorest community cost-to-benefit ratio, indicating uneven progress within the system.Challenges and Broader ContextThe Lown ranking emerged at a critical moment for Ohio hospitals, which are facing inflation, staffing shortages, and possible Medicaid cuts affecting 770,000 residents. MetroHealth, Summa, and UH reported financial losses in 2024, while Cleveland Clinic posted a surplus of $980 million, underscoring regional economic disparities. Despite these challenges, recognized hospitals exemplify how targeted investments in equity and public health can yield positive results. For instance, MetroHealth’s Institute for H.O.P.E. screens patients for social needs like housing and food security, connecting them with local resources, while UH Portage educates families on healthy, budget-friendly eating.The national Lown ranking is led by Duke Regional Hospital in North Carolina, followed by institutions in Tennessee, Texas, and Colorado, reflecting diverse approaches to social responsibility across the country. However, the Lown methodology’s emphasis on fairness and avoidance of overuse contrasts with traditional rankings such as U.S. News, where only two of the top 20 hospitals received an “A” grade for fairness. This gap underscores Lown’s unique perspective, challenging hospitals to rethink their roles as community anchors.Looking AheadAs Northeast Ohio continues to face economic and social challenges, the commitment of these four hospitals — MetroHealth, Cleveland Clinic South Pointe, Summa Health Akron, and UH Portage — serves as a model for others. Their programs, from school clinics to farmers’ markets and educational initiatives, demonstrate that hospitals can be more than healthcare providers — they can be catalysts for change. Yet, criticisms directed at Cleveland Clinic and UH main campuses for inadequate community investments serve as a reminder that even leading systems have room for improvement. In a region where health disparities remain a pressing issue, these institutions stand at the forefront of the battle for a fairer healthcare system — and their efforts may inspire others.
08.07.2025

Health
Massive Recall of Blueberries in Ohio Due to Listeria Threat
Impact on the reputation of organic products: Alma Pak International LLC, a leading supplier of fruits, was forced to recall 12,000 pounds of organic blueberries after the detection of potential listeria contamination. This step, announced by federal health authorities, raised concerns about food safety and highlighted the fragility of supply chains in an era of heightened consumer safety standards.The recall, which the Food and Drug Administration (FDA) classified as the highest risk level — Class I, involves 400 cases of 30-pound frozen blueberries shipped exclusively to a distributor in North Carolina. The product, marked with batch numbers 13325 G1060 and 13325 G1096, was removed after a routine test detected Listeria monocytogenes — a bacteria that can cause serious, and sometimes fatal, illnesses.According to the FDA, none of the batches reached retail store shelves or consumers, and no cases of illness have been reported so far. However, the scale of the recall and its classification as a Class I alert indicate the seriousness of the potential threat. Listeriosis caused by this bacteria poses a particular danger to young children, the elderly, pregnant women, and immunocompromised individuals. In pregnant women, the infection can lead to miscarriages, stillbirths, or premature labor, while in healthy individuals, symptoms typically include fever, headache, nausea, and diarrhea.Alma Pak initiated the recall on June 9, and on July 1, the FDA elevated its status, signaling a "reasonable likelihood" of serious health consequences if contaminated berries are consumed. In a press statement, company representatives emphasized that they have immediately intensified sanitation protocols and monitoring at their facilities. “We take the safety of our customers very seriously,” said Ré.
04.07.2025